Have you ever wondered how pharmacists can do more than just dispense medications? The answer often lies in a collaborative practice agreement. Think of it as a formal partnership between a pharmacist and a physician (or other authorized healthcare provider) that allows the pharmacist to take on expanded responsibilities in patient care. This can include things like adjusting medication dosages, ordering lab tests, and even initiating certain therapies, all under the physician’s oversight and according to a pre defined protocol. It’s a way to improve patient outcomes, enhance access to care, and make the most of a pharmacist’s expertise.
These agreements are especially important in areas where access to doctors is limited or for patients with chronic conditions that require ongoing medication management. Imagine a patient with diabetes who needs regular adjustments to their insulin dosage. With a collaborative practice agreement in place, a pharmacist can make those adjustments in consultation with the patient’s doctor, saving the patient time and a trip to the doctor’s office. It’s a win win for everyone involved.
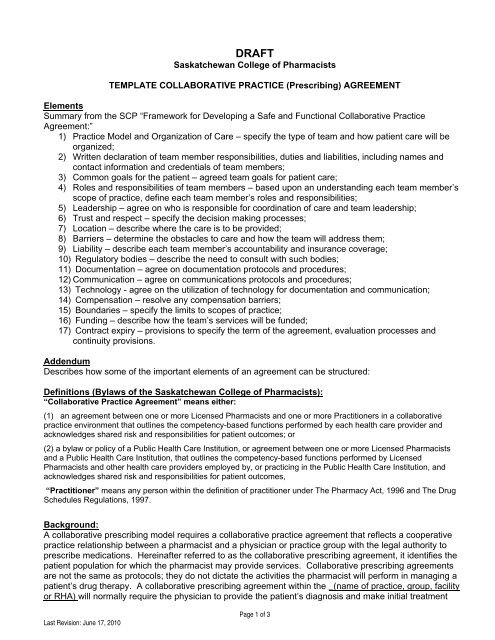
So, how do these agreements actually work? Well, it all starts with a well defined document: the collaborative practice agreement template pharmacist. This template outlines the specific roles and responsibilities of both the pharmacist and the physician, the types of patients who can be managed under the agreement, the medications or conditions covered, and the procedures for communication and documentation. It’s the foundation for a successful and effective collaborative practice.
Understanding the Collaborative Practice Agreement Template
The collaborative practice agreement template is more than just a piece of paper; it’s a detailed roadmap for how the pharmacist and physician will work together to provide optimal patient care. A good template should be comprehensive, covering all the necessary legal and practical aspects of the collaboration. This helps ensure that everyone is on the same page and that the agreement is compliant with state laws and regulations, which can vary considerably.
One of the most crucial aspects of the template is the scope of practice. This section clearly defines what the pharmacist is authorized to do under the agreement. For example, it might specify that the pharmacist can manage patients with hypertension, including adjusting their blood pressure medications and ordering relevant lab tests. The scope of practice should be realistic and aligned with the pharmacist’s training and experience, as well as the needs of the patient population.
The template should also address the procedures for communication between the pharmacist and the physician. How often will they communicate? What methods will they use (e.g., phone, email, electronic health record)? What information needs to be shared? Establishing clear communication protocols is essential for ensuring that the physician is kept informed of the patient’s progress and that any potential problems are addressed promptly. It also provides the structure for quality patient care.
Another important element of the collaborative practice agreement template is the section on documentation. This outlines how the pharmacist will document their activities, including medication adjustments, lab test results, and patient education. Proper documentation is not only essential for patient safety but also for legal and regulatory compliance. The template should specify what information needs to be documented, where it will be stored, and how it will be accessed by the physician and other members of the healthcare team.
Finally, a good template will also address issues such as liability and insurance coverage. Who is responsible if something goes wrong? What type of insurance coverage is required? These are important questions that need to be addressed in the agreement to protect both the pharmacist and the physician. Consulting with a lawyer who specializes in healthcare law is highly recommended to ensure that the agreement is legally sound and protects everyone’s interests. This is especially true when creating a collaborative practice agreement template pharmacist.
Key Elements to Include in Your Collaborative Practice Agreement
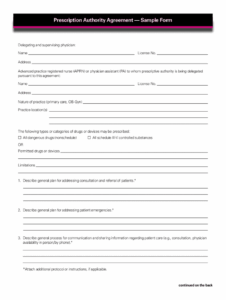
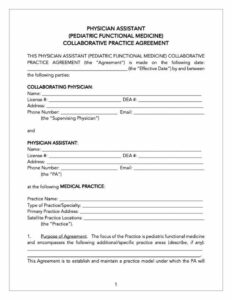
When crafting your collaborative practice agreement, there are several key elements you absolutely need to include to ensure it’s both effective and legally sound. Firstly, clearly define the roles and responsibilities of each party involved. This includes outlining the specific tasks the pharmacist is authorized to perform, the physician’s oversight responsibilities, and the process for making collaborative decisions. Ambiguity can lead to confusion and potential legal issues down the line, so be as specific as possible.
Secondly, establish clear protocols for patient selection and management. This means specifying the types of patients who are eligible for collaborative care under the agreement, the criteria for their inclusion, and the procedures for monitoring their progress. For example, the agreement might state that only patients with stable chronic conditions who are already on established medication regimens are eligible.
Thirdly, address the issue of access to patient information. The agreement should outline how the pharmacist will access the patient’s medical records and other relevant information, while also ensuring that patient privacy is protected. This might involve obtaining patient consent for the pharmacist to access their records or implementing security measures to safeguard sensitive information. Ensure this process meets all HIPAA requirements and any state specific laws.
Fourthly, include a detailed plan for ongoing evaluation and improvement. This should outline how the effectiveness of the collaborative practice will be monitored and evaluated, and how the agreement will be updated as needed. For example, the agreement might specify that the pharmacist and physician will meet regularly to review patient outcomes, identify areas for improvement, and make adjustments to the protocols as necessary.
Lastly, always remember that a collaborative practice agreement should be a living document that evolves over time to meet the changing needs of patients and the healthcare system. It requires ongoing communication, collaboration, and a commitment to continuous improvement. By carefully considering these key elements, you can create a collaborative practice agreement that is both effective and sustainable.
Collaborative relationships between healthcare professionals provide a remarkable opportunity to enhance patient care and outcomes. The use of well crafted agreements is a pivotal step towards unlocking the full potential of these partnerships, ultimately improving lives and optimizing healthcare delivery.
With a clear understanding of the agreement and its important elements, pharmacists and physicians can successfully enhance their collaborative efforts. Ultimately, it allows for better patient care, optimized treatment plans and improved healthcare access.