So, you’re a Nurse Practitioner (NP) ready to spread your wings and practice to the fullest extent of your abilities. That’s fantastic! One crucial piece of the puzzle in many states is the collaborative agreement. Think of it as a roadmap outlining the relationship between you and a collaborating physician. It defines your scope of practice, ensures patient safety, and provides a framework for consultation and support. Navigating the legal landscape of these agreements can feel a little daunting, but with the right information and resources, you can confidently secure a compliant and effective agreement.
What exactly is a nurse practitioner collaborative agreement template, and why is it so important? Well, depending on the state you’re practicing in, these agreements are often a requirement for NPs to practice independently or with a certain level of autonomy. The agreement essentially details the working relationship between the NP and a collaborating physician, outlining the scope of practice, responsibilities, and procedures for consultation and referral. It’s a formal document that helps ensure patient safety and provides a legal framework for your practice.
Imagine it like this: you’re building a house (your practice), and the collaborative agreement is the blueprint. It lays out the foundation, the structure, and the key components that make it all work. Without a clear and well-defined agreement, things could get messy, and you might run into legal or professional challenges down the road. That’s why understanding the ins and outs of these agreements and having access to a reliable nurse practitioner collaborative agreement template is so vital for NPs today. Let’s delve into what makes a good template and how to use it effectively.
Understanding the Essentials of a Nurse Practitioner Collaborative Agreement
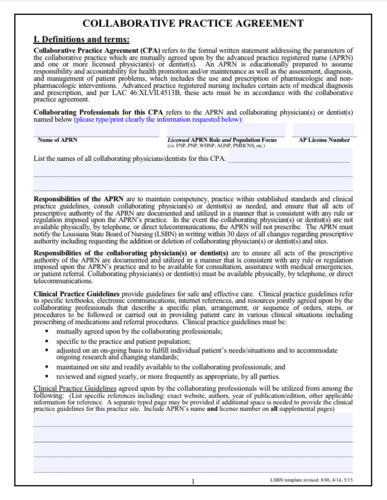
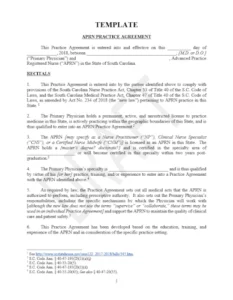
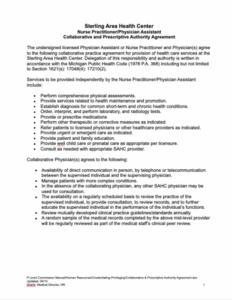
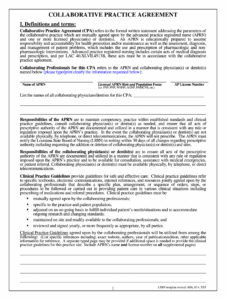
A nurse practitioner collaborative agreement is more than just a piece of paper; it’s a living document that should reflect the unique nature of your practice and the specifics of your state regulations. Each state has its own rules and requirements, so it’s crucial to familiarize yourself with the laws governing NP practice in your location. A good agreement should clearly define the roles and responsibilities of both the NP and the collaborating physician. This includes specifying the NP’s scope of practice, outlining the types of patients the NP can treat, and detailing the procedures the NP is authorized to perform.
Furthermore, the agreement should address the process for consultation and referral. How often will you consult with the collaborating physician? What types of cases require mandatory consultation? What is the procedure for referring patients to specialists or other healthcare providers? These are all important questions that should be answered in the agreement. It should also outline how the collaborating physician will be available for consultation, whether that’s through phone, email, or in-person meetings.
Financial arrangements should also be clearly defined. Will the collaborating physician be compensated for their services? If so, how will they be paid? Will the NP be responsible for covering the physician’s malpractice insurance? Addressing these financial aspects upfront can prevent misunderstandings and conflicts down the road. The duration of the agreement and the process for termination are also crucial elements to include. How long will the agreement be in effect? What are the grounds for termination, and how much notice is required? A well-defined termination clause can protect both parties in the event that the relationship needs to end.
Key Components of a Robust Template
When selecting a nurse practitioner collaborative agreement template, look for one that is comprehensive, customizable, and compliant with your state’s regulations. The template should include sections for defining the scope of practice, outlining the consultation process, addressing financial arrangements, and specifying the duration and termination of the agreement. It should also include clauses related to liability, confidentiality, and dispute resolution.
Remember that a template is just a starting point. It’s essential to tailor the template to your specific practice needs and consult with a healthcare attorney to ensure that the agreement complies with all applicable laws and regulations. Don’t be afraid to ask questions and seek clarification on any aspect of the agreement that you don’t fully understand.
Navigating the Legal Landscape and Ensuring Compliance
One of the biggest challenges facing NPs when drafting collaborative agreements is navigating the complex and ever-changing legal landscape. Laws governing NP practice vary widely from state to state, and what’s acceptable in one state may be prohibited in another. That’s why it’s crucial to stay informed about the latest developments in your state’s regulations and to consult with a healthcare attorney who is familiar with NP practice laws. This legal expert can help you review your agreement, identify any potential compliance issues, and ensure that you are fully protected.
Beyond state laws, you also need to be aware of federal regulations, such as those related to Medicare and Medicaid. These regulations can impact your billing practices, your scope of practice, and your ability to prescribe medications. Failure to comply with federal regulations can result in significant penalties, including fines, exclusion from government healthcare programs, and even criminal charges. Keeping up-to-date on these changes is a must for NPs who wish to maintain a compliant practice.
Another important aspect of compliance is documentation. You need to keep accurate and complete records of all patient encounters, including diagnoses, treatments, and referrals. You also need to document any consultations with the collaborating physician, including the date, time, and subject of the consultation. These records can be crucial in demonstrating compliance with the collaborative agreement and protecting you from liability in the event of a lawsuit.
Furthermore, consider risk management strategies beyond just the collaborative agreement. Maintain adequate malpractice insurance coverage and implement policies and procedures to minimize the risk of errors and omissions. This could include protocols for medication reconciliation, patient education, and follow-up care. Regularly review your policies and procedures to ensure that they are effective and up-to-date.
Remember, ensuring compliance is an ongoing process, not a one-time event. Stay informed, seek legal counsel when needed, and prioritize patient safety in all aspects of your practice.
Ultimately, these agreements are a critical component of NP practice in many states, and a well-crafted agreement can protect both the NP and the collaborating physician, while also ensuring that patients receive high-quality care. Don’t underestimate the importance of taking the time to understand the requirements in your state and to create an agreement that is tailored to your specific practice needs.
Taking the time to do your homework now will save you headaches, money, and potential legal issues in the future, allowing you to focus on what you do best: providing excellent care to your patients. Ensuring that you have the best nurse practitioner collaborative agreement template is a crucial step in building a successful and compliant NP practice.