Have you ever wished your pharmacist could do more to help manage your health? Imagine a world where your pharmacist, working closely with your doctor, could adjust your medication dosages, order lab tests, and play a more active role in your overall care. That’s the power of a collaborative practice agreement, a formal arrangement that expands the scope of what a pharmacist can do.
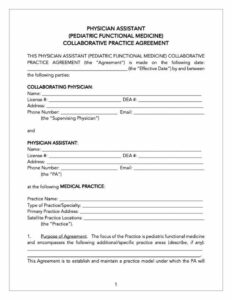
These agreements, often referred to as CPAs, are legally binding documents that outline the specific responsibilities and authorities granted to a pharmacist working in collaboration with a physician or other qualified healthcare provider. Think of it as a roadmap that guides the pharmacist and doctor in providing coordinated and comprehensive patient care. It’s a win win for everyone involved, especially the patient who benefits from increased access to care and personalized treatment.
If you’re a pharmacist or physician looking to establish a collaborative practice, or simply a patient curious about how these agreements work, you’ve come to the right place. We’ll explore the ins and outs of collaborative practice agreements, and guide you to useful information for creating your own pharmacist collaborative practice agreement template. Let’s dive in and unlock the potential of this powerful tool for improving healthcare.
Understanding Collaborative Practice Agreements: A Deeper Dive
Collaborative practice agreements are all about teamwork. They’re designed to foster a strong partnership between pharmacists and physicians, allowing them to leverage their respective expertise to optimize patient outcomes. These agreements aren’t just about convenience; they’re about enhancing the quality of care by enabling pharmacists to take on a more active role in medication management.
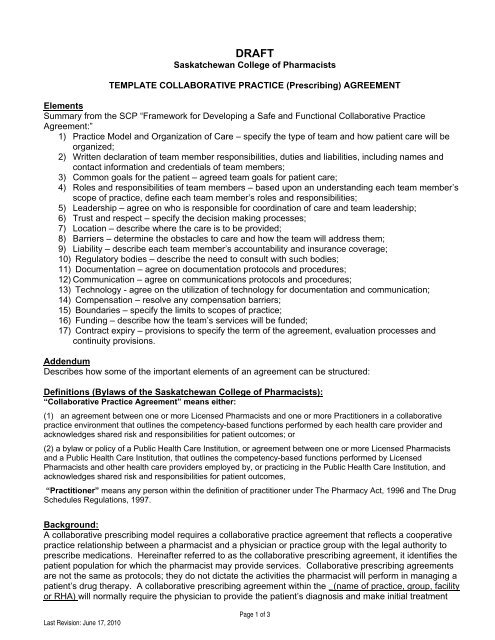
The specific details of a CPA can vary depending on state laws, the types of services offered, and the individual needs of the patients being served. However, most agreements will typically include key components such as the scope of practice authorized for the pharmacist (e.g., adjusting medication dosages, ordering lab tests), the specific patient populations covered by the agreement, protocols for communication and documentation, and mechanisms for quality assurance and review. These agreements really make the partnership more than just a friendly suggestion and make it an actionable plan.
For example, a CPA might allow a pharmacist working in a primary care clinic to manage the medication regimens of patients with hypertension. Under the agreement, the pharmacist could titrate antihypertensive medications based on blood pressure readings, order routine lab tests to monitor kidney function, and provide patient education on lifestyle modifications. This frees up the physician to focus on other aspects of the patient’s care, while ensuring that the patient receives comprehensive medication management services.
It’s important to remember that collaborative practice agreements are not a one size fits all solution. They need to be carefully tailored to the specific practice setting and the needs of the patients being served. A well crafted agreement will clearly define the roles and responsibilities of each provider, outline the procedures for managing potential risks, and ensure that patient safety is always the top priority. If you’re looking for a good starting point, a pharmacist collaborative practice agreement template is the way to go.
The benefits of collaborative practice agreements extend beyond improved patient care. They can also lead to increased efficiency, reduced healthcare costs, and enhanced job satisfaction for both pharmacists and physicians. By working together, these healthcare professionals can create a more seamless and patient centered healthcare experience.
Key Considerations When Developing a Pharmacist Collaborative Practice Agreement Template
Creating a pharmacist collaborative practice agreement template is a significant undertaking, requiring careful consideration of numerous factors. State laws and regulations governing collaborative practice vary widely, so it’s essential to be aware of the specific requirements in your jurisdiction. A template must be fully compliant with all applicable state and federal laws.
Defining the scope of practice for the pharmacist is another crucial step. The agreement should clearly outline the specific tasks and responsibilities that the pharmacist is authorized to perform, such as medication adjustments, lab test ordering, and patient education. It should also specify the patient populations that are covered by the agreement and any limitations on the pharmacist’s authority. Be specific. The vaguer the language, the more potential for misinterpretation.
Communication protocols are also vital for successful collaboration. The agreement should establish clear guidelines for how the pharmacist and physician will communicate with each other, including the frequency and methods of communication. This may involve regular meetings, electronic health record access, or secure messaging systems. Make sure you know how each party can keep the other up to date and stay in communication as needed.
Furthermore, the agreement should address issues related to liability and insurance coverage. It’s important to ensure that both the pharmacist and the physician have adequate malpractice insurance to cover their respective roles and responsibilities under the agreement. The agreement should also specify how liability will be handled in the event of a patient injury or adverse event.
Finally, the agreement should include a mechanism for ongoing review and evaluation. This allows the parties to assess the effectiveness of the collaboration and make adjustments as needed to ensure that it is meeting the needs of patients and providers. Regular review also helps to ensure that the agreement remains compliant with changing laws and regulations. Don’t just make the agreement and then forget it; revisit it frequently!
It’s a system designed to give the best care possible. This system can truly change the dynamic of patient care.
It is important to ensure both parties feel equally represented and understood.